|
Written by Becky Lugardo, PT, DPT Yoga is an excellent way for older adults to loosen and stretch painful muscles, reduce stress, and improve circulation. It also reduces anxiety, helps lower blood pressure, protects joints, and builds strength and balance. Utilizing various modifications to traditional yoga poses and balancing exercises, chair yoga can achieve many of the same health benefits, while significantly reducing the stress on muscles and joints. The chair provides support for traditional standing poses, which are modified to be performed while sitting in the chair. A recent study on Chair Yoga conducted at Florida Atlantic University showed pain reduction, improved mobility and improvement of security and well-being. This 8 – week program was the first to show Chair Yoga as an alternative treatment for lower extremity osteoarthritis. In fact, the Arthritis Foundation recommends yoga to improve joint pain, improve flexibility, balance and reduce stress and muscle tension. A core concept of yoga is to respect your body: be mindful of how your body feels when practicing yoga and accept your physical limitations. Focus on how a pose feels and discern between discomfort and pain. Stop doing any pose that feels painful. As we grow older, our bodies age with us. Healthy lifestyle habits, like regular exercise, can slow the aging process. In addition to regular aerobic exercise, the Physical Activity Guidelines for Americans recommend muscle strengthening activities and exercises to improve or maintain balance. Similar guidelines were jointly released by the American Heart Association and the American College of Sports Medicine, with the addition of flexibility exercises. Research shows a regular exercise program can improve mobility and balance, reduce fall risk and help maintain functional fitness and quality of life. If you are someone who has osteoarthritis, trouble with standing exercise or are just looking for a new low impact alternative to regular exercise, you may want to consider adding a Chair Yoga program into your weekly routine. Yoga adds not only a low impact physical component to your routine, but also a mental one by calming and relaxing participants. Inevitably this can lead to a greater feeling of happiness and well-being…from which everyone can benefit! Give Chair Yoga a Try! We Would Love To See You!Join us as we offer a Restorative Chair Yoga class at CLPT's Shared Studio Space!! Click below to check out the details and register for the class!
1 Comment
 The Fourth of July is right around the corner! When I think of July 4th, I think of fun, family, friends, food, festivities and fireworks. However, the truth is more than 91,000 Americans sustain serious injuries between July 4-5, the highest two-day total for hospitalizations throughout the year. It should come as no surprise that fireworks are the top cause of injuries. More than half of all the fireworks-related injuries sustained by Americans each year occur during the first week of July. Hands and fingers (30%) are the body part most frequently injured by fireworks, as fuses burn faster than advertised, shortening the time for people to move. Injuries sustained from fireworks can include dislocations, broken bones, loss of sight and hearing, disfiguration, amputations, and even death. If you are setting off bottle rockets, rockets, sparklers or any other type of fireworks, always exercise extreme caution. To protect your hands, read and follow all instructions, don’t trust the wick, and stand 500 feet away from the launch site. Aside from fireworks, Independence Day offers ample opportunity for preventable injuries. July’s high temperatures combine with family time, games, swimming, boating, and parades to create a perfect storm for Americans. That is why we compiled some of our top injury prevention tips for you: Good Hydration is Key!Believe it or not, by the time you feel thirsty, the concentration of your blood has already increased by 2%. Proper hydration is essential for a broad range of functions, including increasing brain and digestive function, regulating body temperature and lubricating joints. Heat illness is the enemy of fun, causing fatigue, dizziness and muscle cramps. Without even checking the forecast, it’s safe to assume that Independence Day will be hot near you. In the heat, you’ll expel more fluid through sweat, so it’s more important than ever to fuel up on water. According to the U.S. Institute of Medicine, adults can produce as much as three or four liters of sweat per hour in extreme conditions, so keep the bottle handy and limit alcohol consumption. Backyard Activities Are Fun...But Stretch First!
Don't Be Afraid To Ask For Some Help LiftingWhether you’re transporting a cooler full of chilled drinks, cornhole boards or lawn furniture, don’t lift alone. Grab a family member or friend to help you lift heavy objects, and avoid shoulder injuries, back pain and lumbar injuries. To prevent injuries, always bend at your knees instead of the waist, and lift with your glutes and quads instead of your back and groin. Be Mindful Of Your Posture While preparing food by the grill, sink or counter, stand up to your full height and straighten your back. Keep your knees slightly bent to prevent ankle pain and avoid the risk of fainting. Position your feet shoulder-width apart and distribute your weight more towards your toes, instead of your heels. If you’re sitting to eat, watch fireworks or enjoy a parade, place your feet flat on the ground or a footrest to keep them from dangling unsupported. Always keep your knees at hip-level or below and your ankles out in front of your knees. Avoid crossing your legs, relax your shoulders and ensure that your seat supports your middle and lower back. Our entire team at Crystal Lake Physical Therapy wishes you a safe, happy and healthy 4th of July!!! But if you find yourself sprained or strained on July 5th, don't hesitate to call us to set up a free injury screening or an evaluation! Click here to Schedule
Contributing Author: Holly Schwarz, PT, DPT Summer weather can actually be very helpful in relieving inflammation that contributes to aches and pains! Believe it or not, your summer diet can really help manage inflammation as well! Summer Fruits and Vegetables to Relieve Inflammation
Apricots -Rich in plant-based chemical beta-cryptoxanthin, studies of shown help prevent osteoarthritis as well as inflammatory forms of arthritis. -High in magnesium which strengthen bones and ease pain. Carrots -Beta-carotene lowers uric acid which could help with gout symptoms. -Rich in Vitamin C Watermelon -Contains Vitamin A which helps with bone health. -Beta-cryptoxanthin which may reduce inflammation. -Rich in Potassium and Magnesium which help with elevating bone density. Summer Squash - Antioxidants – Carotenoids, flavonoids, and Vitamin C which help fight free-radical damage and reduce inflammation, slowing cartilage deterioration and reducing joint pain. Cherries -Anthocyanins in cherries help relieve osteoarthritic pain and control gout flares in some people with tart cherries. -Sweet cherries also contain anthocyanins which could help reduce C-reactive proteins, a marker for inflammation in RA and other inflammatory diseases. Tomatoes -Packed with antioxidants, including Vitamin C, Lycopene and Quercetin. -Rich in Vitamin C and A which help lower cardiovascular risk. Additional Ways To Reduce Inflammation1. Eat foods that reduce inflammation as stated above.
2. Lessen sugar intake – sugar can directly cause inflammation. 3. Engage in stress-relieving exercise – mediation, yoga, mindfulness, and light exercise is important with lowering body’s inflammation. You can even go for light walks to help remove inflammation within the body. 4. Add adaptogens to your diet – like ashwagandha or ginseng which are known to stabilize you which help decrease the impact stress has on your body. 5. Sleep more – CDC reports that we do not sleep enough. Lack of sleep reduces the bodies ability to fight infection. 6. Drink adequate amounts of water and stay hydrated. As the weather warms up, many of us are taking the opportunity to get back out in our gardens to enjoy some fresh air, sunshine, and exercise! Whether you are planting new flowers or a vegetable garden, here are some tips to help you have a pain-free gardening experience this year. How To Avoid Knee and Back Pain When GardeningIt is important to think about your body mechanics when you are kneeling, lifting, bending, and squatting while gardening. If you are kneeling, make sure the surface is comfortable for your knees to prevent compression through the kneecap. If needed, put a towel or other soft surface under the knees to cushion them. When bending over, avoid twisting/repetitive motions and avoid staying in this position for too long. Always make sure you are using your legs to lift with good form and to hold any objects close to your body. When squatting down, ensure that you are keeping your knees apart and pushing your butt down and back while engaging your core. If gardening is difficult due to pain with prolonged bending, try using a stool to reduce how far you have to bend down to work. Make sure you get up, move around. and change positions occasionally to prevent stress on the spine. If possible, try working from a raised surface so that you can sit or stand when tired. When lifting, ensure good form and keep your back neutral (no excessive bending or twisting). Preventative Measures You Can Take To Avoid Pain:
If you have additional questions or would like a more personalized assessment, please call or text us at Crystal Lake Physical Therapy to schedule an evaluation. We would love to assist you! (815)893-8480.
October is Breast Cancer Awareness Month. Each year, you see everything from sports teams, pizza boxes, and even police cruisers decked out in pink to help raise awareness. One in eight women will receive a breast cancer diagnosis at some point in her lifetime, and men are not immune. In fact, breast cancer is the second most-diagnosed cancer in women – second only to skin cancer. If you’ve recently received a breast cancer diagnosis, you no doubt have many thoughts, concerns, and questions running through your head. No one wants to endure a mastectomy, but with education, a solid support system, and adequate post-mastectomy physical therapy, you can conquer this hurdle. Here’s everything you need to know about mastectomy recovery and how physical therapy after a mastectomy can make all the difference in the world. What Does Mastectomy Recovery Entail? Cancer treatment in general is physically and mentally challenging in a way people who haven’t experienced it can’t understand. Mastectomy recovery is multifaceted and each woman copes in her own way. Physical recovery from a double mastectomy usually takes between four and six weeks. If you’ve had a radical mastectomy with additional muscle or lymph nodes removed, this can add some length to your recovery time. Furthermore, you’ll need to consider any additional time for reconstruction. Make sure to discuss your options with your doctor and reach out to survivor support networks for advice about deciding whether or not to undergo a reconstruction. Perhaps even more challenging is the emotional aspect of mastectomy recovery. Develop a good support system and allow yourself to experience emotions as they come and go. Can Physical Therapy After a Mastectomy Help Me Recover? Studies show that exercise and physical therapy after a mastectomy are incredibly important for recovery. It’s actually very common for women to develop musculoskeletal issues following a mastectomy and reconstruction because it causes so much disruption to your body’s natural muscle tissue. However, post-mastectomy physical therapy can play a major role in reducing this risk and getting you back to “normal” life as soon as possible. Unfortunately, not enough patients go through with physical therapy after their cancer treatment and mastectomy recovery. In other cases, their post-mastectomy physical therapy isn’t customized. Lack of proper exercise after a mastectomy can lead to muscle loss and poor movement which can add additional strain to your daily life. According to a recent study from the American Society of Clinical Oncology, a personalized physical therapy plan can drastically help you regain your range of motion after the removal of breast tissue and lymph nodes. In their study, women who received comprehensive physical therapy after a mastectomy enjoyed a 32% overall improvement rate post-surgery as opposed to 6% of women who only received education and brochures. This research shows that mastectomy recovery should involve a multifaceted approach with continuous communication between your physical therapist and doctor to reap the full range of benefits. What Can I Expect from Post-Mastectomy Physical Therapy?
Complete recovery is never immediate. It takes dedication and patience. But by channeling your inner strength and coordinating with your physical therapist, you can get ahead in your mastectomy recovery process. Comprehensive post-mastectomy physical therapy will typically involve some of the following modalities depending on your type of surgery and other cancer treatments you’ve had.
Have you recently undergone a mastectomy? At Crystal Lake Physical Therapy, Inc. we are here for you during this difficult and trying time. We want to help you get back to your normal life as quickly as possible. Contact us today to schedule an appointment with one of our women's health specialists! Standing in front of a room full of eager minds providing them with information on your favorite topic can be a very rewarding job. Whether it is teaching preschoolers the colors of the rainbow or college students calculus, most teachers are on their feet for hours at a time. Additionally, small tables and chairs, extra low sinks and toilets, and comfortable floor equipment for story reading have all been designed to fit the needs of our kids. We so often forget that these customized versions of equipment often neglect the fact that the teachers find themselves bending, reaching and modifying their posture to adjust to these tiny ergonomically designed tables and chairs. Bringing knowledge literally down to their level has its consequences. Preserving the health of our teachers is crucial. The fact of the matter is “that two-thirds of workers in primary and early-years classrooms have received treatment for back and joint problems as a result of working in child-sized environments.” A recent study of more than 700 teachers and pre-school staff found that heavy- lifting of children and equipment, using child-height computers and whiteboards, and standing all day were also adding to teachers’ pain. Nearly 40 per cent of those taking part in the study had taken time off work because of work-related joint or back pain. So what can you do as a teacher to avoid these injuries?!? Here are some tips for reducing low back pain:
“ I have some problems with a little urine leakage, but I have had two kids, so this is normal.”  These are common statements that are often heard from patients in our clinic. While the occurrence of urinary incontinence is common among seniors, it must not be regarded as a normal aging side effect. It is a problem that can be successfully addressed and treated! According to the National Association for Continence 25 million Americans have issues with incontinence. Only 1 in 12 people will seek medical advice about it; perhaps because it is an uncomfortable issue to talk about, or possibly because of the belief or acceptance that it is a normal part of growing older. The fact is urinary incontinence is costly: economically, psychologically and physically.
Causes of Incontinence The causes of incontinence can vary from an urinary tract infection to something more complex associated with a chronic medical condition.
Types Of Urinary Incontinence  Stress Urinary Incontinence This type of incontinence occurs secondary to weakness of the core muscles and fascial connections around the bladder. The pressure on the bladder causes leakage during coughing, sneezing, laughing, and during exercise. It can also occur when lifting or bending over. Urgency Incontinence This type of incontinence is associated with urgency and an overactive bladder (OAB). There is a strong, sudden urge to urinate. The bladder contracts and an involuntary loss of urine occurs. Overflow Incontinence This type of incontinence occurs due to an overflow of urine in the bladder. This can be due to a blockage at the urethra such as an enlarged prostate, poor sensation of the bladder, or the nerves to the bladder are affecting the ability of the bladder to empty completely. Functional Incontinence A person may have normal bladder control, however physically cannot make it to the restroom in time. Regardless of which type of incontinence a person may have, nonsurgical management, such as physical therapy, is the first line of treatment. Physical Therapy For Incontinence Bladder Retraining Bladder retraining involves different aspects depending on the issues/needs of the patient
Pelvic Floor Muscle and Core Training The coordination of the pelvic floor and abdominal muscles is very important to continence. It is not just about doing kegels, but coordinating the entire core and postural system.
The bottom line is that non-invasive treatment options in physical therapy are extremely beneficial and successful in addressing symptoms associated with urinary incontinence. In other words, there is NO reason that you should just expect urinary leakage to be a normal part of your life! Especially when you can address these symptoms often in as little as 3 weeks with targeted exercise and training!
For more information or to schedule an appointment to see a pelvic floor physical therapist, please click below. Healthcare for moms is ripe for a revolution. Currently in the United States, postpartum checkups occur around 4-6 weeks after childbirth and only last about 10 minutes. You may have a brief pelvic examination, talk about future birth control plans, and likely get an “all clear” from your doctor, stating you can return to activity as usual. This means sex, exercise, and work. And that is your postpartum care. No more follow ups. No discussion of common pelvic floor conditions women experience. No discussion about steps to take if problems arise. Chances are you will not have your abdomen assessed for diastasis recti, a separation of your abdominal muscles that commonly occurs during pregnancy. You may feel and look like you are still pregnant and your diastasis will not be diagnosed. You may have pelvic floor problems like urinary leakage, painful sex, or pelvic organ prolapse and not know that diastasis recti and pelvic floor dysfunction often go hand in hand. You may not know that the crunches you are doing to get your abs back after the baby could be making this condition worse. And you may have no idea that pelvic physical therapy can help. Yup, you’re good. All clear. Chances are you will not have your pelvic floor muscles tested by your doctor to assess for weakness or spasm. You may go back to running and leak urine. You may do jumping jacks and feel heaviness in your vagina like something is falling out. You may start yoga, which you hear is great for postpartum recovery and have embarrassing vaginal farts. You may get on a spin bike or stair stepper and have excruciating tailbone pain. And you may have no idea that any of this may be due to weak or tense pelvic floor muscles and pelvic physical therapy can help. Yup, you’re good. All clear. Chances are you will not have a conversation with your doctor about returning to sex and the discomfort or pain many women experience after childbirth. Healing tissue from a vaginal tear or episiotomy may cause a pain with penetration during sex and maybe even cause some bleeding afterwards. Your vagina may be very dry, you can’t orgasm, or you may leak urine when you orgasm. And you have no idea that pelvic physical therapy can help, so you just bear through the pain or avoid sex altogether. Yup, you’re good. All clear. Chances are you won’t receive education on how to massage your C-section scar. You have bladder problems, groin pain, or constipation all stemming from your scar tissue restriction. You can’t wear jeans anymore, you avoid lying on your stomach, and you don’t like wearing your baby in a carrier because your scar hurts. And you have no idea that pelvic physical therapy can help, so you just deal with it. Yup, you’re good. All clear. Women’s bodies go through incredible physical, hormonal, and musculoskeletal changes during pregnancy and childbirth. As a pelvic health physical therapist, I have worked with women during pregnancy and the postpartum period for over a decade. I help educate them how to care for their pelvic floor muscles, inform that that any pain, leakage, or prolapse is not normal. I guide them on a safe return to exercise, sex, and activity to meet the increasing demands of their lives. Time and time again I hear, “I had no idea this type of physical therapy existed” or “why didn’t my doctor tell me about this sooner.” The postpartum care for women is in desperate need of improvement and the awareness of pelvic physical therapy needs to grow. Pelvic Physical Therapy should be standard care for every postpartum woman in the United States. I am baffled that medical professionals send sleep-deprived women home with bleeding vaginas, tender scars, sore breasts and a newborn baby to care for – and all they get are - Yup, you’re good. All clear. This was originally posted on The Vagina Whisperer by Sara Reardon Pelvic Floor Physical Therapy is covered by your insurance!
If you are postpartum (even if you had your last baby 50 years ago or more!!) click below to schedule your appointment today! Kegels. We all know the word. But do we really know what it actually, truly MEANS to do a Kegel, and why do we even care? I will tell you. And believe me, I have a love/hate relationship with the Kegel, which I will explain.
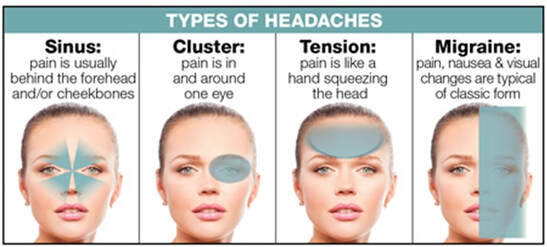
We have Dr. Arnold Kegel to thank, back in 1948 for coming up with the famous “Kegel” exercise. He was a gynecologist, and was looking for a non surgical way for women to help “tone” the pelvic floor muscles to help with urinary leakage after they had a baby. I don’t hate him for it. Being a physical therapist, I want all things conservative first, and YAY for starting with exercise. Good on ya, Dr. Kegel! This opened up a new view on trying to help women after childbirth with staying dry, which is a great step forward in the ever-challenging path of providing comprehensive care for women postpartum (which I am sad to say, leaves something to be desired in this country). However, Kegel’s became the blanket approach for EVERYONE who reported any sort of bladder or bowel or pelvic dysfunction. Pain with sex? Kegel. Leaking urine? Kegel. Having increased urge and going to the bathroom all the time? Kegel. Back pain? Kegel. Pregnant? Kegel And the list goes on…. However, I am here to tell you that kegels are not the answer to everything, and although they are appropriate for some people, they are not appropriate for all, and should not be thought of as such. Mind blown. I know. Stay with me. A kegel is a concentric, or shortening action, of the pelvic floor muscles, which sit at the bottom of your pelvis. They lie like a basket, or a hammock, and attach front to back (pubic bone to tailbone) and side to side (sit bone to sit bone). Within these muscles, we find openings. In females, we have the rectum, the vagina, and the urethra. In men, we have the rectum, and the urethra follows the length of the penis and is past the pelvic floor, where it ends at the tip of the penis. The pelvic floor has 3 main functions: 1) Support (holds us and our organs up against gravity) 2) Sexual (aids in orgasm and allowing vaginal penetration for women) 3) Continence (keeps us dry). In a perfect world, as the bladder and rectum are filling with urine and stool, the pelvic floor muscles “turn on” to close the sphincters that hold in the urine and stool. We get the signal to either head to the restroom to pee or grab our phones for some reading material if we are going in for a longer stretch. The pelvic floor muscles then lengthen, or relax, and the bladder muscle (the detrusor) pushes urine out through an open urethra, all thanks to a relaxed and lengthened pelvic floor. Now, if the muscles have lost a bit of strength, maybe say...I don’t know, going out on a limb here….holding a baby, plus weight, the placenta, organs, gravity, increased fluids, etc, FOR 9 MONTHS, in addition to the force of actually pushing a baby out, AND the need to lengthen and stretch to get out of the way to make way for the baby….we may see a bit of an issue with holding in urine, or stool. Not to mention if there was any perineal or pelvic floor muscle trauma or prolapse sustained during delivery! So yes, in this case, it is a good idea, probably, to strengthen your pelvic floor by way of the Kegel. HOWEVER, in some cases, these muscles can be too short, or too contracted, and adding more contractions on top of an already contracted, or too short muscle, isn’t always the best idea. Think about trying to do a bicep curl when you’re already curled….the elbow isn’t going anywhere, and all that extra curling will prob make your bicep hurt! Another issue I have with blindly prescribing Kegels...and we’ve all heard this: “Just do 200 kegels a day” or “ do your kegels while sitting at a stop light”... is that not everyone’s baseline level of strength and function is the same. Also, we don’t go to the gym and do 200 bicep curls everyday, or walk around carrying a 35lb pound weight with our bicep all day every day. We shouldn’t be prescribing set parameters without assessing. Because some people, may not need to do Kegels, in fact they may need to work on lengthening or stretching their pelvic floors. These muscles can be too short or tight, and oftentimes Kegels will, and can, make some symptoms and dysfunction worse. There have been studies published in the literature that looked at women who were instructed to perform Kegel’s and like 30% of women don’t contract their pelvic floor at their first consult. So..bottom line is this: if you’re not sure, ask for help. Find a pelvic floor PT (yours truly) to assess and get you on the right track. Performing a Kegel the correct way is really hard, actually. The pelvic floor muscles have to work with a host of other muscles AND your breath AND be effective like all the time to keep us supported and continent. It’s not easy to get this contraction going correctly, and I’ve had high level athletes who have crazy body awareness have a really hard time getting a correct Kegel. So there you go. Kegels are important, for sure, but in the right context, with the right person and situation. Click below to schedule an appointment today. We can help you get that pelvic floor muscle working the way it should! In the US over 37 million people suffer from migraines or chronic headaches. For many, headaches can be disabling, with chronic headache sufferers being three times more likely to suffer depression as well. There is a treatment beyond medications that has been proven to help decrease the occurrence of headaches–physical therapy. Unfortunately most headache sufferers have never been told about this possibility. Physical therapy including exercise, relaxation techniques and posture retraining have been shown to be as effective as many medications in decreasing the frequency of headaches. In order to understand how physical therapy can help alleviate headache pain we must first look at the two main types of headaches. Cervico-genic headaches, or tension headaches, are the most common type of headaches. Secondly and often more debilitating are migraine headaches. Tension Headaches
Tension headaches are caused by referred pain from the muscles of the neck and the base of the head. Most people may know about referred pain during a heart attack, when pain is referred into the right arm. This is the same mechanism that can cause headaches when the muscles in the neck are extremely tight or unbalanced. Let’s take a look at what a large majority of Americans do for most of the day: sit at the computer. When we sit slumped over the computer, the muscles of the neck–mainly the upper trapezius, the sternocleidomastoid and the suboccipital muscles at the base of the skull–all become extremely tight and over worked. This tension can cause pain and stiffness in the neck as well as refer pain to the head. Physical therapy can first relax the tension in the muscles with soft tissue mobilization or massage and joint mobilization which decreases acute pain. Exercises are then given to help strengthen the neck and postural muscles to allow these muscles to withstand the tensions of day to day life. Finally, posture retraining and relaxation techniques can help decrease extraneous tension on these same muscles to help the patient continue to manage the symptoms after discharge from physical therapy. Migraine Headaches The rational for physical therapy treatment of migraine headaches is a little more complex. Migraines are a “centrally mediated” pain. This means the central nervous system is involved. We know that migraines are caused by a trigger that causes a change in the way the cranial nerve 5 or the trigeminal nerve interacts with the brain stem. The trigeminal nerve is the same nerve that also regulates sensation to the face and is responsible for TMJ functions of biting and chewing. For this reason we know that treating TMD (temporomandibular joint dysfunction) can lessen the frequency of headaches. Furthermore, the fibers of the upper cervical spine that regulate the neck muscles meet with the trigeminal nerve in an area of the brain called the trigeminocervical nucleus. Because of this convergence of the nerves, the neck muscle dysfunction can now become a trigger of the trigeminal nerve and cause a migraine. Treating the neck as mentioned above can be very effective in alleviating the pain of a migraine and decreasing frequency of the occurrence for many sufferers. If you suffer from migraines or chronic headaches, there may be help. Physical therapy is a very safe and cost effective treatment of headaches that might just be the answer for you. Call us today or click below to schedule an appointment for a personalized evaluation. |
AuthorEmily Craigen, owner of Crystal Lake Physical Therapy, is a Doctor of Physical Therapy and a local Crystal Lake resident who is excited to bring health and wellness to her community. Archives
August 2023
Categories |
- Home
- About Us
-
What We Treat
- Arthritis
- Balance and Gait Disorders
- Back Pain and Sciatica
- Chronic Pain
- Elbow, Wrist and Hand Pain
- Fibromyalgia
- Hip and Knee Pain
- Incontinence
- Motor Vehicle Accident Injuries
- Multiple Sclerosis
- Neck Pain
- Pelvic Pain
- Pre-Surgical Rehab
- Post Surgical Rehab
- Shoulder Pain
- Sports Injuries
- TMJ Dysfunction
- Vestibular Rehab
- Work Injuries
- Myofascial Release
- MPS/Dolphin Neuro Stim
- Become A Patient
- Contact Us
- Blog
- Workshops
- Patient Resources
















 RSS Feed
RSS Feed